The macula, the center region of the retina that is crucial for clear, detailed vision, is the place where abnormal blood vessel formation under the retina leads to wet macular degeneration. Although the precise reason for this abnormal growth is not fully understood, it is believed to be a result of a number of genetic, environmental, and lifestyle factors.
Wet macular degeneration causes
Wet macular degeneration has a number of risk factors, including age, smoking, a family history of the condition, high blood pressure, and obesity. The sun’s UV rays, a diet high in saturated fat, and a history of cardiovascular disease are among the additional variables that may raise the risk of developing wet macular degeneration.
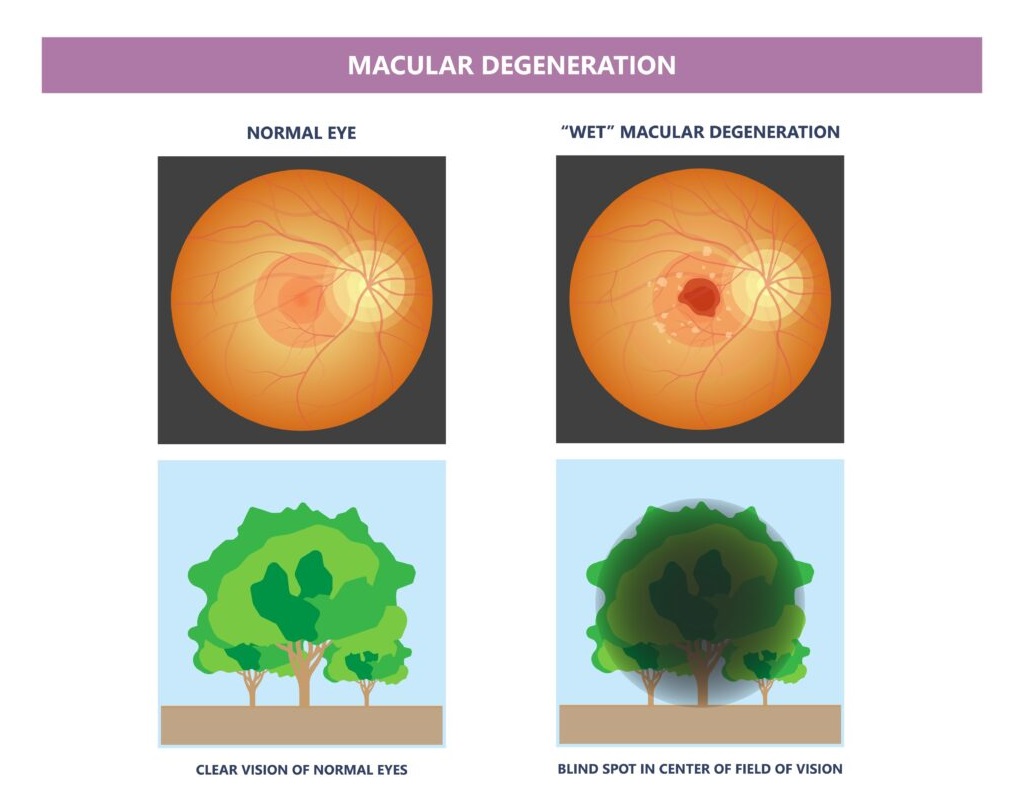
The macula can become damaged and lose vision if aberrant blood vessels that are growing beneath the retina in the macula start to leak fluid, blood, and other substances. This may cause blurred or distorted vision, a blind spot in the center of the field of vision, and trouble focusing on minute details.
How do the cells in our eyes age?
The eye’s cells alter as we age in a number of ways that may impair our vision. Here are a few examples:
- Age-related presbyopia (difficulty seeing up close) and cataracts (lens clouding) can both be brought on by the eye’s lens becoming less flexible and transparent.
- Age-related macular degeneration (AMD), which can impair central vision, is caused by a steady decline in the retina’s cell structure.
- Cornea: As people age, their corneas may thicken and become less transparent, which might impair their ability to see clearly.
- Iris and pupil: As we age, the muscles in the iris and pupil may weaken, making it more challenging to react to variations in light levels.
- Optic nerve: As we age, the optic nerve may experience changes that impact how visual information is transmitted to the brain and may result in diseases like glaucoma.
These changes collectively have the potential to cause a loss in visual acuity, contrast sensitivity, color vision, and other visual abilities as we age. To identify and treat age-related eye diseases early, it is crucial to have routine eye exams.
How the Macular Cells Age and can be the Cause of wet macular degeneration?
Age-related macular degeneration (AMD), a prevalent cause of vision loss in older persons, has an unknown specific cause. However, scientists have identified a few essential causes of the macular cells’ degeneration, including:
Waste product accumulation
Over time, the macula’s cells can accumulate waste materials, which may result in the creation of drusen, which are deposits. These drusen can obstruct the macular cells’ normal function and speed up their aging.
Oxidative stress
Oxidative stress can destroy the cells of the macula and contribute to AMD when the formation of dangerous molecules called reactive oxygen species (ROS) outpaces the body’s capacity to neutralize them.
Inflammation
Prolonged eye inflammation can potentially speed up the macular cells’ deterioration. Smoking, high blood pressure, and obesity are a few examples of variables that may contribute to this inflammation.
Genetics
Some genes have been found to enhance the likelihood of getting AMD, indicating that genetic factors may also contribute to macula degeneration.
All in all, these elements have the potential to harm the macula’s cells, especially the photoreceptor cells that are in charge of detecting light and transmitting visual information to the brain. Central vision may become distorted, hazy, or lost entirely as these cells age.
How High blood pressure can cause wet macular degeneration?
The lack of oxygen can harm the blood vessels in the eye and promote the abnormal growth of blood vessels under the retina, which is a defining feature of wet macular degeneration, high blood pressure (hypertension) can lead to wet macular degeneration.
The walls of the blood vessels may thicken and become less flexible as a result of high blood pressure, which can reduce blood flow to the eye and harm the retinal blood vessels. By causing damage, the body can produce growth factors that encourage the creation of aberrant blood vessels in the macula, which can then leak fluid and blood and cause wet macular degeneration.
Additionally, conditions like atherosclerosis (hardening and narrowing of the arteries), stroke, and other illnesses that may advance wet macular degeneration can all be made more likely by hypertension.
Therefore, lowering high blood pressure through medication and/or lifestyle modifications can aid in lowering the risk of developing wet macular degeneration and other complications related to the eyes. To maintain their eye health and identify any changes that may need therapy, people with hypertension should have regular eye exams.
How smoking contributes to wet macular degeneration?
Smoking is a well-known risk factor for wet macular degeneration, and it is believed to do so through a number of different pathways that contribute to the onset and development of the condition.
The blood vessels in the eye, including those in the macula, might get damaged as a result of smoking. Wet macular degeneration may result from this injury because it may trigger inflammation and the growth of new blood vessels, which may allow fluid and blood to leak into the macula.
Smoking can cause oxidative stress, which happens when the body’s capacity to neutralize dangerous chemicals known as free radicals is outpaced by the rate at which they are produced. Oxidative stress can harm the macula’s cells and play a role in AMD development.
Immune system impairment: Smoking can negatively impact immune system performance, which increases the risk of infection and inflammation in the eyes. AMD development may be accelerated by eye inflammation.
Smoking can cause a reduction in blood flow to the eyes, which may accelerate the onset and progression of AMD.
Generally speaking, smoking is a big modifiable risk factor for wet macular degeneration and quitting can greatly lower the risk of contracting the condition. Quitting smoking can assist those who already have wet macular degeneration decrease the disease’s progression and lower their risk of developing further visual loss.
Wet macular degeneration caused by saturated fat?
There is conflicting information regarding the link between the consumption of saturated fat and wet macular degeneration. While other studies have not found a strong correlation, some have suggested that a diet high in saturated fat may increase the risk of developing AMD.
Nevertheless, a diet rich in saturated fats can also increase the risk of other diseases like obesity, hypertension, and high cholesterol, all of which are known risk factors for AMD. For instance, consuming a lot of saturated fat can cause blood vessels to accumulate cholesterol, which can exacerbate atherosclerosis (the hardening and constriction of the arteries). Reduced blood flow to the eye caused by atherosclerosis can harm the retinal blood vessels and cause AMD.
Saturated fats can also add to the body’s chronic inflammation, which is thought to be a factor in the emergence of AMD. Chronic inflammatory conditions can harm retinal cells, especially those in the macula, and promote the development of atypical blood vessels.
However, it is generally advised to eat a healthy, balanced diet low in saturated fat to lower the risk of developing other conditions that can hasten the onset and progression of AMD. Overall, the evidence linking saturated fat intake to wet macular degeneration is inconclusive.
How inflammation can contribute to wet macular degeneration?
It is believed that inflammation significantly contributes to the onset and progression of wet macular degeneration. Chronic inflammation in the eye can harm the macula’s cells, encourage the development of aberrant blood vessels, and worsen wet macular degeneration’s hallmark leakage of blood and fluid into the retina.
Among the ways that inflammation might cause wet macular degeneration are as follows:
Damage to cells
The photoreceptor cells in the macula, which are in charge of detecting light and transmitting vision information to the brain, are susceptible to damage from chronic inflammation. The function of these cells may be hampered by this damage, which may also contribute to the onset of AMD.
Blood vessel growth that is abnormal
Inflammation can encourage the creation of growth factors that support the growth of blood vessels that are abnormal in the macula. These blood vessels have the potential to leak fluid and blood, harming the macula and accelerating the onset of wet macular degeneration.
Immune system impairment
Because of immune system impairment caused by chronic inflammation, the eyes may be more vulnerable to infection and inflammation. AMD development may be accelerated by eye inflammation.
Accumulation of waste material
Chronic inflammation can also contribute to the buildup of waste materials in the macula’s cells, which can result in the development of drusen, or deposits. The macular cells may become degenerated as a result of these drusen interfering with their normal operation.
Overall, it is believed that chronic inflammation plays a substantial role in the onset and development of wet macular degeneration. The progression of the disease may be slowed down and eyesight may be preserved by reducing inflammation by dietary changes and/or medicines.
Symptoms of Wet Macular Degeneration
Depending on the degree and stage of the disease, wet macular degeneration can produce a wide range of symptoms. The following are some typical signs of wet macular degeneration:
- Vision distortion or blurriness: People with wet macular degeneration may have distortion or blurriness in their central vision, making it challenging to read, identify people, or carry out other jobs that call for precise, clear vision.
- The center of a person’s visual field may develop dark or empty patches as a result of wet macular degeneration, making it challenging to see items in that area.
- Wet macular edema patients may notice changes in their ability to see colors, such as a reduction in color intensity or a shift in color perception.
- Straight lines appear wavy or crooked: Straight lines can appear wavy or crooked due to wet macular degeneration, which can be an obvious sign when reading or seeing a grid pattern.
- People with wet macular degeneration may find it difficult to adjust to low-light conditions, such as when entering a dark room or driving at night.
- Rapid onset of symptoms: Wet macular degeneration can occasionally cause symptoms like distorted or blurry vision or a sudden loss of central vision to appear suddenly and quickly.
Treatment of Wet Macular Degeneration
There are treatments that could perhaps halt the growth of the disease and protect existing vision. Early treatment has the potential to restore some lost vision.
Medications
Anti-VEGF medications have been shown to be effective in preventing the development of new blood vessels. These drugs prevent the body’s growth signals from causing the production of new blood vessels. For all stages of wet macular degeneration, they are regarded as the first line of treatment.
Treatment options for wet macular degeneration include:
- Avastin (bevacizumab).
- (Lucentis) Ranibizumab.
- Eylea (Aflibercept).
- Beovu (brolucizumab).
- Vasbysmo (faricimab-svoa)
These medications are injected into the troubled eye by your ophthalmologist. To sustain the therapeutic impact of the medication, you could require shots every 4 to 6 weeks. As the blood vessels contract and your body absorb the fluid under the retina, you might occasionally regain some vision.
Photodynamic treatment
The irregular blood vessel growth in wet macular degeneration may be treated with this therapy. It is far less frequent than anti-VEGF injection therapy, though.
Your eye doctor administers verteporfin (Visudyne), a medication, via an injection into an arm vein during photodynamic therapy. After then, the medication enters the blood vessels in your eyes. Your eye doctor uses a specialized laser to direct concentrated light to the problematic blood vessels in your eye. Due to the verteporfin being activated, the issue blood vessels shut. The leak is stopped by this.
Your eyesight may be enhanced and the pace of vision loss may be slowed down by photodynamic therapy. Because the treated blood vessels might reopen, you might require additional treatments in the future.
You must stay out of the sun and bright lights after photodynamic therapy until the medication has left your body. This could take several days.
Photocoagulation
Your eye doctor will use a high-energy laser beam during photocoagulation therapy to close off problematic blood vessels under the macula. In order to lessen future harm to the macula, this technique aids in stopping the bleeding from the arteries. Blood vessels may grow again after this treatment, necessitating subsequent therapy. Scarring brought on by the laser may also result in blind spots.
Wet macular degeneration patients are rarely treated with this method. If you have problematic blood arteries just beneath the macula’s center, it’s usually not a possibility. Additionally, the likelihood of success decreases the more damaged your macula is.
Low vision rehabilitation
Your side vision is unaffected, and age-related macular degeneration does not result in complete blindness. But it can diminish or even take away your central vision, which is essential for driving, reading, and identifying faces. You might benefit from receiving care from an occupational therapist, an expert in low vision rehabilitation, your eye doctor, and others. They can assist you in figuring out how to adjust to your shifting eyesight.
FAQ’s
Can lost vision with wet macular degeneration be restored?
A wet AMD. When anti-VEGF antibodies are injected into the eye, lost vision in people with wet AMD, which is brought on by new, leaky blood vessels sprouting into the retina, can occasionally be restored.
Is it possible to stop wet macular degeneration?
A crucial step in preventing AMD is to stop smoking or never start. Maintaining a healthy lifestyle and reducing cholesterol will reduce your risk of developing AMD and help stop the dry type of the illness from developing into the wet form, which can result in irreversible vision loss.
Wet macular degeneration: what causes it?
Wet AMD is a less frequent form of late AMD that typically results in a rapid visual loss (also known as advanced neovascular AMD). Wet AMD can develop at any stage of dry AMD, however wet AMD is always the late stage. The macula suffers damage when aberrant blood vessels develop behind the eye.